Stop Dieting in 2024…and why it is ok.
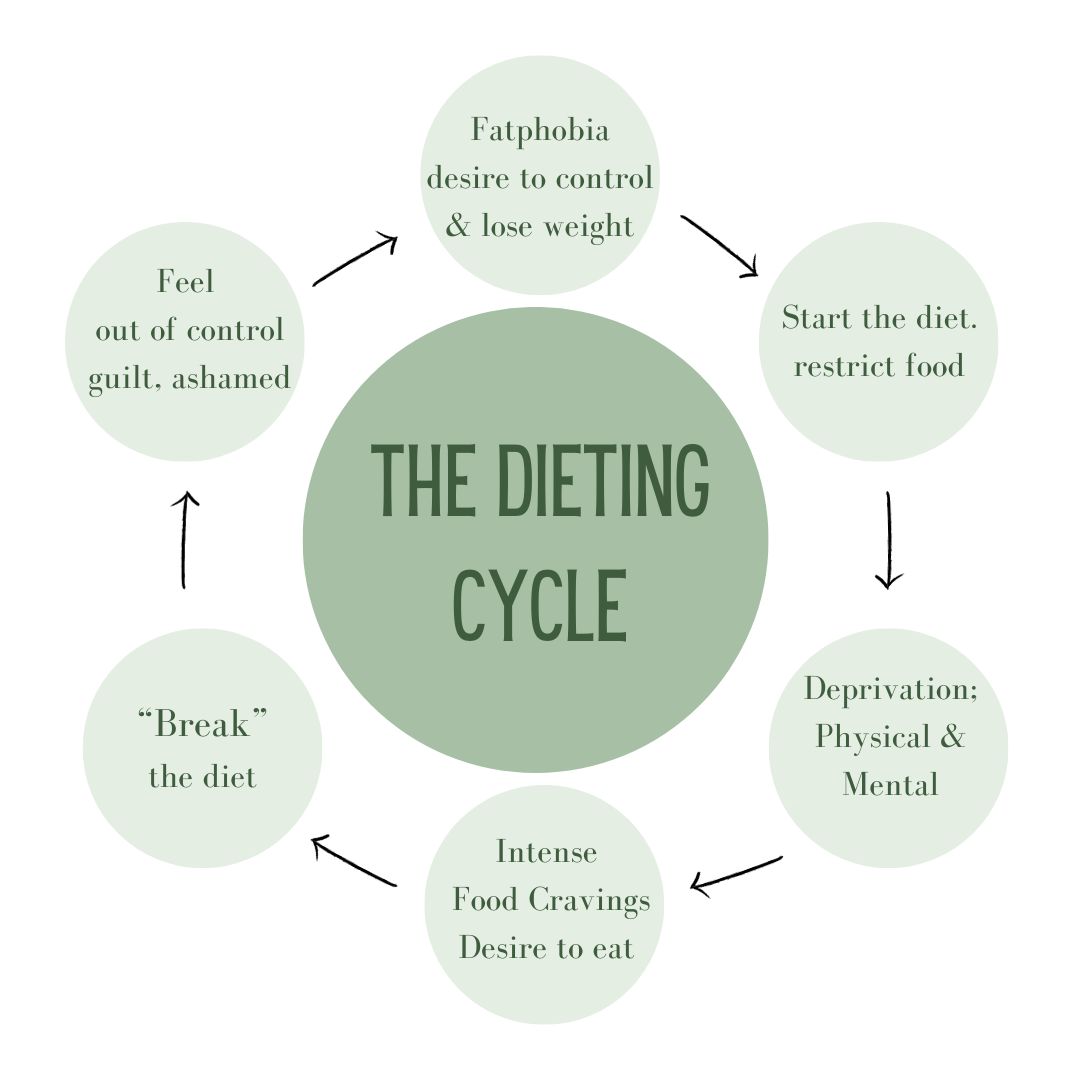
We all know New Year’s resolutions don’t work. And yet, there it is, the little voice whispering “maybe this year.” Maybe this time I can finally lose the weight, for good. I just need to be stronger, find the right plan, follow the right influencer, join a gym…and so on. Consider the image below, does this resonate with you?
Alyssa Rumsey, MS, RDN, CDN, CSCS- modified
Ultimately my question is why? Why, are so many of us having this conversation? Why, after decades of battling “obesity” are more Americans gaining weight at the same rate the dieting industry is growing? (1) Because the problem is not you, it’s the diets.
Let me say that again…IT IS NOT YOU that is the problem.
We are told that shrinking our body is the only path to health, vitality, and acceptance. That is unacceptable.
The truth is, restriction in the name of health has been around for centuries, with fad diets taking hold at the end of the 19th century. The public policy shift in the 1990’s and medicalization of “obesity” in the early 2000’s ramped up funding agendas and conversations in healthcare and schools.
Also, small caveat. Can we talk about the word “obesity?” It stems from the Latin word obesus, meaning “having eaten itself fat.” I think that sums up the lens from which we are viewing this issue.
Yes, when it comes to body size and health we’ve got research (mountains of research), but to me, the view feels a bit narrow. I think we are missing some fairly big gaps in the narrative.
First, the bulk of the research is epidemiological. Epidemiologic research is designed to illustrate associations. Or, in other words, that two variables are somehow related, not that one variable necessarily causes the other. Yet, the narrative remains: “high BMI causes chronic disease.” We need to dig deeper.
Second, confounding variables (2) such as physical inactivity (3), socioeconomic status, mental health, environmental exposures, or access to healthcare are largely not considered in the research. It is time to start taking a look at how these, and others, may be impacting health if body size is a constant.
I’m not suggesting the current research is invalid. I think we can acknowledge the proposed risk of carrying extra weight (4) and metabolic imbalance, while still challenging the current diet paradigm. I am not anti-weight loss, I am anti-dieting. Bodies change throughout our life cycle and in various situations; we are not meant to be stagnant. But, the narrow focus on lowering the number on the scale brings its own share of harms that are often downplayed in “obesity” research. These include a high rate of weight regain, a risk for fat overshooting, weight cycling (yo-yo diets), metabolic adaptation, an increase in obsessive thinking, binge behavior, eating disorders, and a decrease in self-esteem and self-trust. (5,6,7,8,9,10,11,12,13) I suspect that these points do little to improve overall stress and inflammation, which are reliable factors of chronic disease.
“Diet culture is a system of beliefs that equates thinness to health and moral virtue. It promotes weight loss as a way to obtain higher status and demonizes certain ways of eating while elevating others. It masquerades as health, wellness, and fitness and for some, it is all consuming. ”
The pressure to weigh less has infiltrated not just our media and homes, but our healthcare system, schools, and relationships. It is undeniably present in our daily conversations with patients around health and nourishment. This is why so many of us in dietetics and healthcare are starting to stand up and challenge the current system.
In my opinion we need a paradigm shift away from “You are fat and it is your moral and civic responsibility to fix the problem.” This suggests that you are broken, that you have complete control over your body’s physiology, that you have total access to all you need to make changes, and that health is not available to you if you have a diagnosed condition. I propose a shift. Encourage embodiment. Widen the lens on what impacts a person’s metabolism, overall health and behaviors. Let the individual decide what aspects of “health” feel right.
A weight inclusive approach is just that. Step out from behind the goal of weight loss and diet culture to get clarity on what “health” looks like for you. When you shift from weight-centric to weight inclusive approaches, you start to look at life-enhancing and self-care behaviors that support your health(14) instead of merely the number on the scale. A non-diet approach is about allowing flexibility and enjoyment around eating while developing the confidence and self trust needed to make decisions that are right for your body.
So, what would a non-diet approach look like for you in 2024? Do you feel there are areas in your life that need adjustments? If not, you can stop here. Keep living your life as you choose. If so, I encourage you to start small and take the time to consider your what, why, how, and where.
1) What areas of self-care need your attention?
Sleep
Movement
Stress management
Meal planning, cooking, nutrition education
Body respect
Medical care or following up with a doctor you trust
Social connection
Spirituality
Any others that come to mind?
2) Why is change, in this area, important to you?
3) What are some specific actions you can start, this week, to address your self-care choice?
Lastly, look for ways you can support the changes you are trying to make. This can be as simple as switching up your daily routine, voicing your needs to a loved one, or reaching out to a weight inclusive provider for help. The truth is change is hard and it takes time. Be patient with yourself, this is all about you and your health journey. Give yourself permission to so slow down, enjoy the process, and end the diet cycle for good!